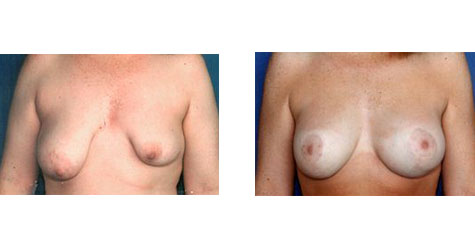
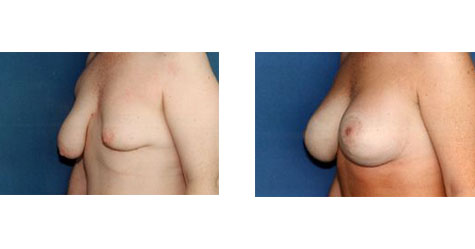
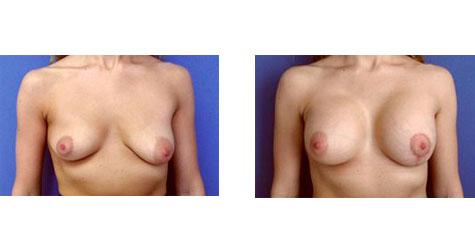
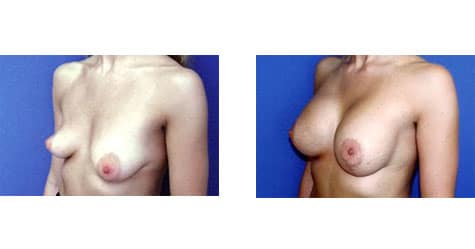
Asymmetrical Tuberous Breasts Conveniently located to serve Pittsburgh and Pennsylvania
Women with asymmetrical tuberous breasts require extra care and attention in order to bring the size and shape of their breasts into harmony with one another. Creating symmetry can enhance a woman’s appearance tremendously. Because of this, Dr. Cherup takes the time to thoroughly examine and treat each breast augmentation patient using the latest technology.
She uses an advanced system to precisely measure the tuberous breasts and chest wall according to a number of parameters. Careful measurement and analysis allow her to determine the most appropriate size implants for each individual patient to correct for their asymetric tuberous breasts. Dr. Cherup is in a unique class of Pennsylvania surgeons who use this precision measuring system to ensure their patients receive the best results possible.
View our gallery of before and after results! Or, schedule your consultation with Dr. Cherup.

-
Post Operative Care
Position:
During the first week, attempt to sleep on your back instead of on your side. We want your implants to stay in a perfect position during the initial healing process. This is not a “life and death” issue, however. If you cannot sleep on your back, sleep in another comfortable position.
Activity:
Avoid heavy lifting and straining for two weeks minimum. You may, however, do normal activities at any time if they cause no pain or discomfort. Let your body tell you what you can do or not do.
Dressings:
The bra acts as a “dressing,” holding the breasts and implants in perfect position. Try to keep the bra “even.” If the bra feels too tight or hurts, switch immediately to any bra that feels comfortable. A bra that is too tight can cause ulceration of the skin – YOU MUST NOT LET THIS HAPPEN! We want you to wear a bra at all times for 2 weeks. After 2 weeks, you may sleep without the bra. You should not go braless during the day for 4-6 weeks after surgery. It is probably more comfortable not to wear an underwire bra.
Showering and bathing:
You may shower the day after surgery. If you prefer to bathe, do not allow the incision lines to soak for more than a few minutes in the bath water. Leave the adhesive strips (steri-strips) on your skin. (Do take your bra off while you bathe).
Sutures:
Our doctors will remove the sutures below your skin 10-20 days after surgery.
Exposure to sunlight:
Scars take at least one year to fade completely. During this time, you must protect them from the sun. Even through a bathing suit, a good deal of sunlight can reach the skin and cause damage. Wear a sunscreen with a skin-protection factor (SPF) of at least 15 at all times when in the sunshine. Be extremely careful if areas of your breast skin have reduced sensitivity.
Exercise:
You may take gentle walks within a few days. Do not return to aerobic exercise for 3 weeks.
Driving:
You may drive when driving does not cause pain. This usually occurs in 4-6 days if you have a car with power steering.
Specific As You Heal Information
Activities
It is important that you not engage in strenuous activities in the first 3 weeks after surgery. Aerobic exercise will raise your blood pressure, which could cause late bleeding and harm your result. If your job keeps you sedentary, you may return to work when you feel comfortable, several days after surgery. Once you begin exercising again, start gently and let your body tell you what it can tolerate. Don’t rush! !
Healing of sensory nerves:
Regeneration of the sensory nerves is accompanied by tingling, burning, or shooting pains, which will disappear with time and are nothing to be alarmed about. If however, this is accompanied by swelling or redness, infection, or bleeding, then you will need to see one of our doctors at the office.
Asymmetry:
It is quite common for the two breasts to heal differently. One may swell more, one may feel more uncomfortable, or the shapes may differ initially. After complete healing, they should look remarkably similar and natural. Patience is required, but if you are concerned, ask questions of Dr. Cherup or the nursing staff.
“Sloshing” sensation:
You may hear and feel “sloshing” in your breast after surgery. This is not the implant! It is the air that is trapped in the space around the implant and the natural fluid that accumulates after an operation. It will all be absorbed by the body within a few weeks.
Shiny skin:
The skin of your breasts may become shiny. This is a result of the swelling that occurs after surgery. Within a few weeks, the edema and swelling will subside and the skin will look more normal.
Sensitivity:
As the nerves regenerate, the nipples commonly become hypersensitive. This will subside with time. You may find that gentle massaging helps.
-
Surgical Risks
Capsular Contraction:
Capsular contraction is the most common “complication” or side effect of breast implant surgery. During surgery, a pocket is created for the implant that is somewhat larger than the implant itself. During healing, a fibrous membrane called a capsule forms around the device. Under ideal circumstances, the pocket maintains its original dimensions and the implant “rests” inside, remaining soft and natural. For reasons still largely unknown, however, the scar capsule shrinks or contracts in some women and squeezes the implant, resulting in various degrees of firmness. This contraction can occur soon after surgery or many years later and can appear in one or both breasts. Current theories suggest that a low grade infection may “trigger” some contraction. The use of a textured surface on the implants seems to alter the way in which the scar capsule develops. Although use of textured implants has not eliminated capsular contraction, it appears to have reduced this risk to the 5-10% range.
Capsular contraction is not a “health” risk, but it can detract from the quality of the result and cause discomfort, pain, or distortion of the breast contour. In cases of minor contraction, we usually will not suggest surgical correction. Cases of very firm contraction may require surgical intervention. Rarely, if the contraction recurs and cannot be eliminated, the occasional patient may choose to have the implants permanently removed.
Hematoma:
Some postoperative bleeding into the pocket containing the breast implant occurs in 2-3% of women. If the bleeding is minimal, the body will absorb it with time. Marked swelling will probably require surgical removal of the blood, in the O.R. or sometimes by a radiologist.
Infection:
Postoperative infection is uncommon, but possible. We reduce this to a minimum by giving intravenous antibiotics during surgery and oral antibiotics after surgery. Most infections are mild and resolve without incident. If a serious infection develops, the implant will probably need to be removed, and cannot be safely replaced for at least 2 months after healing.
Loss of Sensation in the skin or nipples:
Nerves that supply skin or nipple sensation may be cut or damaged while the pocket or space for the implant is being created. Although this does not happen routinely, it can happen no matter how carefully the surgery is performed. If sensory loss occurs, the nerves slowly recover over a period of 1-2 years in about 85% of cases.
Exposure or extrusion of implant:
Thin skin, inadequate tissue coverage, capsule formation, infection or severe wrinkling may all contribute to the erosion of an implant through the skin or scar. Should this very rare complication occur, implant removal would probably be indicated (at least temporarily).
Wrinkling:
With the use of textured implants, visible wrinkling under the skin has been more noticeable. Occasionally, the edge of the implant can be felt. These problems are usually mild and require no treatment. Experience has shown that the wrinkles frequently improve or even disappear within a year. (See Subpectoral Placement below.)
Asymmetry:
If your breasts had slightly different shapes before surgery, they may remain slightly different after surgery. Rarely, in spite of careful attention to detail, the dissected pockets may end up slightly different in shape or height. If this is not noted while you are in surgery, but becomes a problem after healing, you may later need a small adjustment procedure.
Subpectoral placement of the implant (placement under the muscle):
If you and Dr. Cherup have decided to place the implants under the pectoralis muscle, a unique set of risks apply. During contraction of the muscle, the implants will temporarily be flattened and/or pulled upward. Occasionally, the implants may “ride” higher than their original position because of the muscular contraction. Implants were originally placed under the muscle to reduce the frequency of capsular contraction. With the use of textured implants, the frequency of capsular contraction appears to be the same as when the implants are placed above the muscle. Implants are usually placed under the muscle in thin, small- breasted women to provide more “cover” over the implant. Placing the implants under the muscle may reduce visible wrinkling.
Deflation:
If for any reason the valve or implant covering fails, the saline will leak and be excreted by your body. This causes no medical harm, but the implant will need to be replaced in a secondary procedure. The rate of saline-implant leakage is quoted at about 1% over many years.
Loss of skin, breast tissue, or nipple:
This is an extremely rare complication of breast enlargement. It usually develops from an infection that has gotten out of control and results in the death of the involved tissues. This very rare complication will usually involve only small areas that will eventually heal with good wound care. Secondary surgery is a remote possibility.
Interference with breast feeding:
Many women with breast implants have nursed their babies successfully. Nevertheless, any breast surgery can theoretically interfere with your ability to breast feed.
Calcium deposits in the tissue or around the implant:
In some patients, a thin layer of calcium will develop within the scar capsule surrounding the implant. This usually occurs several years after the implant has been inserted. In these patients, the added density of the scar may reduce the detectability of lesions close to the scar on mammograms. Breast cancers may still be visible and detectable when specialized techniques are used.
Breast Cancer:
There is no evidence linking implants and breast cancer. The only clinical studies available show that the prevalence of breast cancer in women with implants is the same or even slightly lower than that in women without breast implants! Furthermore, two studies have shown, to date, that the stage of breast cancer detection in women with implants appears to be identical to that found in the overall population.
Interference with mammography:
You should alert the technician to the fact that you have implants. Special techniques will be used and extra views may be needed in order to see as much of the breast tissue as possible. Even under the most ideal circumstances, some breast tissue may remain unseen and a suspicious lesion missed. Because the breast is compressed during mammography, it is possible, but rare, for an implant to rupture.
Synmastia (loss of cleavage):
This is a very unusual problem that can develop after normal augmentation either above or below the muscle. The skin over the lower sternum (breastbone) pulls away from the bone, and normal cleavage is reduced or eliminated. In its more serious form, the pockets on either side merge to form a single pocket. In the more minor form, the pockets remain separate, but the skin tents upward. Reduced fibrous or elastic “strength” in the subcutaneous tissues may be contributory but is difficult to predict. If the problem develops, correction will require secondary surgery.
Immune disorders:
Some women have claimed that silicone gel prostheses have contributed to or stimulated connective tissue disorders such as systemic lupus erythematosis, scleroderma, rheumatoid arthritis etc. Other complaints involving the nervous system, skin and immune systems have been reported. Reports claiming a causal relationship between silicone gel and such symptoms have been published in the medical literature and widely reported in the press. To the present time, no such relationship has been established scientifically. Gel implants are not available for routine use because of the concerns of the Food and Drug Agency. The saline (salt water) used to fill saline implants is harmless and is excreted in the urine should the implant leak or rupture.
Presence of silicone rubber:
Saline-filled implants are made of silicone rubber. Although silicone rubber has not been implicated in any diseases, and has been used in many types of implants, its use is under investigation.
Breast augmentation is an elective procedure. Enlargement of the breast with fat transfer is not an acceptable procedure. Chest wall muscle exercises may be minimally helpful.
Schedule a Consultation
For more information on treating your asymmetric tuberous breasts in Pittsburgh, PA, contact surgeon Lori L. Cherup M.D. at her main office in Pittsburgh, Pennsylvania.
Call Dr. Cherup at (412) 220-8181 or (877) 441-0639 or use our online form below.
You Might Also Be Interested In…
Dr. Lori Cherup also provides:
From Our Patients…
“Dr. Cherup and her entire staff made me feel comfortable and safe through their professionalism and confidence in their work. We spoke about my wants and desires for what I wanted after surgery and why. We chose the best course of action for me, together. I am thrilled with my results and have been sharing my positive experience with everyone I know. I couldn’t be more pleased with the decision to get this surgery done, but even more so that I chose the best Surgeon and team to preform it.”